I read in yesterday’s newspaper (yes, I am old enough to still read printed newspapers) that obesity is a key link to the soaring costs of health care in the United States. Americans who are 30 or more pounds overweight added an estimated $147 billion in weight-related medical bills to health care costs nationwide in 2008, according to a study presented Monday at a meeting sponsored by the Centers for Disease Control and Prevention to discuss ways to reduce obesity.
The average American is 23 pounds overweight. Multiply that by the number of Americans, and you get 4.6 billion pounds of fat.
And an awful lot of type 2 diabetes, which is what leads to much of the increase in medical costs. The aggregate economic cost of obesity in the United States is estimated to be in excess of $60 billion per year.
So it seems like a good week for us to take a look at weight, why we gain it, and how we might lose it.
Am I fat? Are You?
Obesity is, in simplest terms, excessive body fat. How much is too much? The best way to measure obesity is to determine a person’s buoyancy by measuring their body weight under water. Perhaps you won’t be surprised to learn that this isn’t done very often. Instead, a more convenient statistical estimate is used called the body-mass index (BMI). The BMI is your weight in kilograms divided by the square of your height in meters.
By correlating BMI values with medical records, doctors have concluded that anyone with a BMI of 25 or more is overweight, with increased risk of medical complications. The risk goes way up for people with a BMI of 30 or more, who are defined as obese.
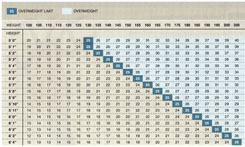
So how are you doing? To see if you have a BMI of 25 or more, use the table below (it saves you having to convert pounds to kilos and feet to meters). I am six feet tall and weight 182, so my BMI comes in at 24. Whew!
As a Nation, How Are We Doing?
If the average American is 23 pounds overweight, it stands to reason our nation has a problem with its weight. When the BMI of Americans is measured, half have a BMI of at least 25, and fully one-third of the population has a BMI of 30 or more.
Are We In an Obesity Epidemic?
There has been a dramatic increase in people with a BMI of 30 or more in recent years, from 15% in 1980 to 23& in 1994, to 34% in 2006 (the latest numbers available). In pervious columns I have trumpeted this dramatic increase in high-BMI individuals as a sign of an obesity epidemic, and most public news sources have as well. However, we do well to cock a careful eye, as whether this is truly an epidemic depends on how one looks at the data. Variation in body weight is a continuous trait (that is, if you lined a thousand people up according to their body weight, you would get a bell-shaped curve, with the mean value at the top), whereas obesity is a fixed threshold. A small shift in the trait’s mean value can lead to a huge increase in the number of people who exceed the threshold. Thus the 33% increase in obesity in the 1990s was associated with an average weight gain of only 3 kilograms (six and a half pounds) in the whole population.
This small shift in America’s body weight, while hardly an epidemic, has had profound effects on our nation’s health, and the cost of maintaining it.
So Why Are We Getting Fatter?
What has lead to the 3 kilo increase in American body weight in recent decades? In a nutshell, we are eating a lot more food rich in calories and fat. A burst of recent books point the finger of blame for this squarely at the food industry, claiming they deliberately manipulate sugar and fat content to encourage consumption.
I suspect they are right. But there is more to the story than that. Our bodies are designed to resist the effects of such meddling with our eating instincts. Each of our bodies has an elaborate system that balances fat with body mass, a system that evolved long ago when humans were hunter-gatherers. Too little fat would put a person at risk of starvation, too much would increase the risk of predation and disease.
Our weight control system is based on a hormone called leptin. As your or my body weight increases, fat tissues secrete higher levels of leptin. This hormone then travels through the bloodstream to the brain, where it binds to leptin receptors in the hypothalamus and other regions to produce a sensation of satiety and so a decrease in food intake. Conversely, a reduction in body weight lowers leptin levels and increases food intake. The result? You and I tend to maintain a relatively constant weight, regardless of how much we eat.
Severe obesity results when you disable this system. Mice with mutations in the ob gene (the gene that encodes leptin) fail to produce leptin and show a five-fold increase in body fat. Humans with mutations in this gene or in the one encoding the leptin receptor similarly become massively obese. So genes also play a big role. When identical and non-identical twins are compared, the heritability of obesity (the percentage of variation due to genetic factors) ranges between 70% and 80%, a very high number. The only human trait with a consistently higher number is height.
So both genes and environment (what you eat and how much of it) play a role. Some of us apparently many of us — are genetically predisposed to obesity, but don’t actually become obese unless we are induced to overeat.
Why Should We Bother to Diet?
This conclusion is actually very good news. While our leptin system will prevent us from losing large amounts of weight, it is quite practical to loose on the order of five to ten pounds by diet and exercise, and this amount of weight loss can have a major impact on your health (remember the bell-shaped curve discussed above).
And What’s This About Health Care Costs?
Of course, a lot of Americans are more than ten pounds overweight. So if our legislators are truly interested in reducing the nation’s health costs, they should get aggressive in pushing anti-obesity therapy. For example, emerging data indicate that leptin (a long-acting hormone from fat tissue) interacts extensively with another hormone called amylin (a short-term signal from the stomach) to control appetite. In preliminary studies, leptin and amylin together induce substantial weight loss in laboratory animals. Studying the efficacy and safety of this combined therapy in humans should be a high priority. More on alternative approaches next week.
© Txtwriter Inc.